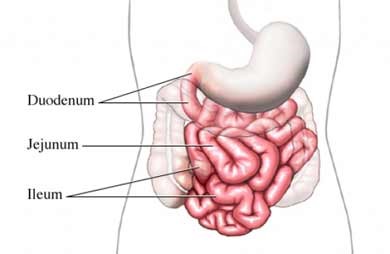
Crohn's disease, named after Dr. Burrill B. Crohn, who was a member of the team that first described the disease in 1932, belongs to a group of conditions known as inflammatory bowel diseases (IBD). Crohn’s disease is a chronic inflammatory condition of the gastrointestinal (GI) tract. It causes inflammation, ulcers, and bleeding in the digestive tract. Crohn’s usually affects the end portion of the small intestine called the ileum, but any part of the digestive tract can be affected, from the mouth to the anus.
Small Intestine
Copyright© Nucleus Medical Media, Inc
What causes Crohn’s disease?
According to the Crohn’s and Colitis Foundation1, Crohn’s disease may affect as many as 780,000 Americans. The cause of Crohn's disease is not known, but inflammatory bowel diseases, such as ulcerative colitis and Crohn's disease, seem to run in families. Some researchers think that it is due to a reaction to a virus or bacteria that causes the immune system to overreact and damage the intestines.
Types of Crohn’s Disease
There are 5 types of Crohn’s disease that impact different parts of the digestive tract. Different symptoms and complications may be associated with each. The 5 types of Crohn’s disease are:
- Ileocolitis
The most common form of Crohn's, ileocolitis affects the end of the small intestine (the ileum) and the large intestine (the colon). Symptoms include:
- Diarrhea
- Cramping or pain in the right lower part or middle of the abdomen
- Significant weight loss
- Ileitis
This type affects only the ileum. Symptoms are the same as ileocolitis. In severe cases, complications may include fistulas or inflammatory abscess in the right lower abdomen.
- Gastroduodenal Crohn's disease<
This type affects the stomach and the beginning of the small intestine (the duodenum). Symptoms include:
- Loss of appetite
- Weight loss
- Nausea and vomiting
- Jejunoileitis
Jejunoileitis is characterized by patchy areas of inflammation in the upper half of the small intestine (the jejunum). Symptoms include mild to intense abdominal pain and cramps following meals, as well as diarrhea. In severe cases or after prolonged periods, fistulas may form.
- Crohn's (granulomatous) colitis
This type of Crohn’s disease only affects the colon. Symptoms include:
- Diarrhea
- Rectal bleeding
- Disease around the anus (abscess, fistulas, ulcers)
- Skin lesions and joint pains are more common in this form of Crohn's than in others.
Crohn’s Disease vs. Ulcerative Colitis
| Crohn’s Disease | Ulcerative Colitis |
|---|---|
| Inflammation may develop anywhere in the GI tract from the mouth to the anus | Limited to the large intestine (colon and rectum) |
| Most commonly occurs at the end of the small intestine | Occurs in the rectum and colon, involving a part or the entire colon |
| May appear in patches | Appears in a continuous pattern |
| May extend through entire thickness of bowel wall | Inflammation occurs in innermost lining of the intestine |
| About 67% of people in remission will have at least 1 relapse over the next 5 years | About 30% of people in remission will experience a relapse in the next year |
Risk Factors
A risk factor is something that increases your chance of developing a disease or condition. Risk factors for Crohn’s disease affect men and women equally, and include:
- Being of Jewish heritage.
- Family history of inflammatory bowel disease or other autoimmune diseases.
- Being between the ages of 15 and 35.
Symptoms
Symptoms of Crohn’s disease often flare up and then go into remission2. Symptoms may include:
- Diarrhea
- Abdominal cramps and pain
- Rectal bleeding
- Weight loss
- Fatigue, weakness
- Nausea
- Fever
- Mouth sores
- Sores, abscesses in the anal area
- Antibiotics
Complications of untreated Crohn's disease may lead to:
- Fistulas—abnormal connections between the intestine and other organs or tissues, such as the bladder, vagina, or skin
- Intestinal obstruction
- Liver disease
- Bowel perforation
- Bleeding
- Kidney stones
- Gallstones
- Osteoporosis
Diagnosis
You will be asked about your symptoms and medical history and a physical exam will be done. If you are diagnosed with Crohn's disease, testing can be used to monitor the disease and assess complications.
Tests may include:
- Blood tests
- Stool tests
Imaging tests evaluate the intestines and surrounding structures, and may include:
- Upper gastrointestinal series
- Lower gastrointestinal series
- Flexible sigmoidoscopy
- Colonoscopy
- CT scan
- MRI scan
- Ultrasound
- X-ray
A biopsy may be taken during some of these tests. A biopsy is a sample of the intestinal tissue that can be examined under a microscope.
What are the treatment options for Crohn’s disease?
There is no cure for Crohn’s disease, but several treatment options that can help ease the symptoms and stave off flare ups. After a diagnosis, recommended treatment may include:
Dietary Changes
Your doctor may advise that you avoid foods that trigger symptoms. These foods are different for each person. They may include:
- Dairy foods due to lactose intolerance
- Highly seasoned foods
- High-fiber foods
Medications
>There are many types of medications that are used to treat Crohn's disease, including:
- Aminosalicylates, a class of medication used to treat Crohn’s disease and ulcerative colitis
- Anti-inflammatory medications that reduce inflammation in the digestive tract
- Immune modifiers, also called immunotherapy, that use the body’s own immune system to fight disease or infection
- TNF inhibitors
- Antibiotics
Surgery
Very severe Crohn's may not improve with medications, and the diseased section of the intestine may need to be removed. The two remaining healthier ends of the intestine are then joined together. You are still at high risk for the disease returning.
Surgery also may be done if you have an obstruction or fistulas.
Prevention
Exercise may help reduce the risk of developing Crohn's disease. Talk with your doctor about an exercise program that is best for you.
Resources
For additional information and to connect with other people who have Crohn’s disease, visit the Crohn’s and Colitis Foundation at http://www.crohnscolitisfoundation.org/ or the National Institutes of Health at www.niddk.nih.gov.
Sources:
1Crohn’s and Colitis Foundation: http://www.crohnscolitisfoundation.org
2National Institutes of Health - Crohn's Disease: www.niddk.nih.gov
If you are exhibiting symptoms of Crohn’s Disease, please consult your physician. Dr. Shail Sheth, with Regional Health Gastroenterology can help with diagnosis and treatment. To schedule an appointment call the office at (812) 234-5400 or click below to book an appointment online.