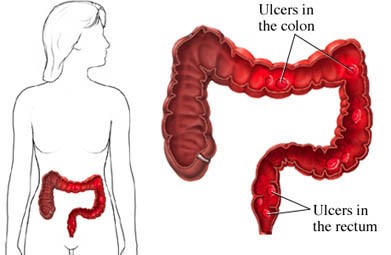
Ulcerative colitis (UC) is a type of severe, chronic inflammatory bowel disease (IBD) of the large intestine, also called the colon, which affects about 700,000 Americans each year1. UC causes:
- Inflammation in the lining of the colon and rectum.
- Ulcers that produce pus and mucous in the lining of the colon and rectum.
- Bleeding in the lining of the colon and rectum.
Ulcerative Colitis
It is important not to confuse an inflammatory bowel disease (IBD) like ulcerative colitis or Crohn’s disease with irritable bowel syndrome (IBS)2. IBS is a disorder that affects the muscle contractions of the bowel and is not characterized as a chronic disease with intestinal inflammation.
Ulcerative colitis is closely related to Crohn's disease because both are types of IBDs that involve inflammation of the digestive tract:
| Ulcerative Colitis | Crohn’s Disease |
|---|---|
| Limited to the large intestine (colon and rectum) | Inflammation may develop anywhere in the GI tract from the mouth to the anus |
| Occurs in the rectum and colon, involving a part or the entire colon | Most commonly occurs at the end of the small intestine |
| Appears in a continuous pattern | May appear in patches |
| Inflammation occurs in innermost lining of the intestine | May extend through entire thickness of bowel wall |
| About 30% of people in remission will experience a relapse in the next year | About 67% of people in remission will have at least 1 relapse over the next 5 years |
Causes of Colitis
The exact cause of ulcerative colitis is unknown. A virus or bacteria may cause the immune system to overreact and damage the colon and rectum.
Risk Factors
A risk factor is something that increases your chances of getting a certain disease or condition. Risk factors for developing ulcerative colitis are relatively unknown, but having a family member with IBD (including UC and Crohn’s disease) may increase your risk of developing UC.
Symptoms
Symptoms and complications of ulcerative colitis affect men and women equally, most often developing between the ages of 15-30. Symptoms may include:
- Diarrhea
- Abdominal cramps and pain
- Rectal bleeding
- Anemia
- Weight loss
- Fatigue, weakness
- Nausea
- Fever
- Skin rashes
- Arthritis
- Eye inflammation, such as uveitis
Intestinal complications of UC may include:
- Perforation, a hole in part of the wall of the gastrointestinal tract
- Fistula—abnormal passageway between 2 bodily structures
- Obstruction
- Excess bleeding
- Toxic megacolon—a potentially life-threatening condition when the colon severely expands and can result in reduced blood flow
Other complications of UC may include:
- Liver disease
- Kidney stones
- Osteoporosis
- Colon cancer
The major symptoms of ulcerative colitis include abdominal pain and bloody diarrhea. When the disease becomes severe, individuals may develop fever, weight loss, dehydration, and anemia. Sometimes, constipation develops instead of diarrhea. Arthritis, skin sores, and liver inflammation may occur, as well. One of the most feared consequences of ulcerative colitis is dramatic dilation of the colon, which can lead to fatal perforation of the colon. Ulcerative colitis also leads to a greatly increased risk of colon cancer.
UC tends to wax and wane, with periods of remission punctuated by severe flare-ups. Medical treatment aims at reducing symptoms, and achieving and maintaining remission.
Diagnosing UC
Testing may include:
- Blood tests
- Stool test
- Barium enema
- Flexible sigmoidoscopy
- Colonoscopy
- Biopsy
Treatment Options
Treatment options may include:
Dietary Changes
Your doctor or dietician can help determine which foods may work best for you. Some foods that they may recommend avoiding are:
- Dairy (due to lactose intolerance)
- Alcohol
- Red and processed meats
- Refined sugar
- Saturated fat
Medications
There are a range of medications that may be prescribed, such as:
- Aminosalicylates
- Steroid anti-inflammatory medications
- Immune modifiers
- Biological agents
Surgery
Surgery involves partial or complete removal of the colon. It is curative and reduces the risk of colon cancer. Surgery may be necessary for:
- An emergency, such as a perforation, excessive bleeding, or life-threatening infection
- Long-term disease that does not respond to medications or other treatment
- Colon cancer—includes confirmed diagnosis or suspicious tissue on examination
- Lack of growth because of nutritional deficiencies (in children)
Other Natural Treatments
People with ulcerative colitis can easily develop deficiencies in many nutrients. Chronic bleeding leads to iron deficiency. Malabsorption, decreased appetite, drug side effects, and increased nutrient loss through the stool can lead to mild or profound deficiencies of protein, vitamins A, B-12, C, D, E, and K, folate, calcium, copper, magnesium, selenium, and zinc. If you have ulcerative colitis, supplements to restore adequate body stores of these nutrients can improve specific symptoms and overall health. Other supplements to consider include:
- Essential Fatty Acids—may help to reduce symptoms of UC
- Probiotics—good bacteria that helps keep the digestive tract healthy
- Aloe—may be beneficial in attaining full or partial remission of UC symptoms.
- Curcumrin / Tumeric – may help in reducing inflammation caused by ulcerative colitis
Be aware that some herbs and supplements can interact adversely with drugs used to treat ulcerative colitis. Be sure to consult your healthcare provider before taking any supplemental treatments.
Prevention
There are no current guidelines to prevent ulcerative colitis. It is a chronic, lifelong condition that requires ongoing treatment.
Resources
For additional information and to connect with other people who have ulcerative colitis, visit the Crohn’s and Colitis Foundation - www.crohnscolitisfoundation.org.
Sources:
1Crohn’s and Colitis Foundation: www.crohnscolitisfoundation.org
2: Crohns and Colitis:www.crohnsandcolitis.com/ulcerative-colitis
If you are exhibiting symptoms of ulcerative colitis, please consult your physician. Dr. Shail Sheth, with Regional Health Gastroenterology can help with diagnosis and treatment. To schedule an appointment call the office at (812) 234-5400 or book an appointment online below.