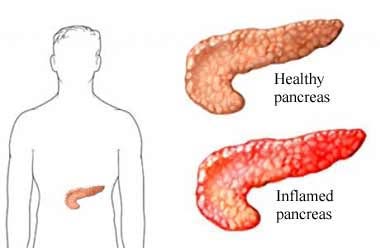
The pancreas is a long, flat, pear-shaped organ that sits behind the stomach and creates enzymes necessary to break down starch, protein, and fat. In addition, cells responsible for creating insulin are found in the pancreas. The enzymes pass from the pancreas, through a duct, to the small intestine. The enzymes are normally not active in the pancreas. Pancreatitis is a condition in which the pancreas becomes inflamed. When pancreatitis is prolonged, pancreatic function declines, leading to malabsorption of nutrients and, possibly, mild diabetes.
Types of Pancreatitis
Pancreatitis occurs in three forms:
- Acute (short-term) pancreatitis
- Recurrent acute pancreatitis
- Chronic pancreatitis
Causes of Pancreatitis
Acute Pancreatitis
Acute pancreatitis is a painful condition, but with treatment it ordinarily resolves in 3 to 7 days. Causes include:
- Alcohol abuse
- Gallstones
- Extremely high blood levels of triglycerides
- Direct trauma to the pancreas
- Abdominal surgery and related procedures
- Kidney failure
- Poor blood flow to the pancreas
- Infection
- Certain medications, such as those that treat high blood pressure or cancer
Recurrent Pancreatitis
Recurrent pancreatitis involves multiple bouts of acute pancreatitis, sometimes in a more mild, prolonged form.
Chronic Pancreatitis
Chronic pancreatitis is a more gradual process that leads to partial or complete pancreatic failure. Its most common causes are:
- Alcohol abuse
- Injury or chronic infection
- Drug or toxic exposure
- Autoimmune disease
- Blockage of the pancreas
In some cases, chronic pancreatitis is genetic and has no known cause.
Symptoms
Symptoms of pancreatitis may happen once or occur many separate times. A flare up of symptoms is known as an attack. Symptoms may include:
- Severe pain in the center of the upper abdomen
- Pain may spread into the upper back
- Pain is made worse by eating, walking, or lying down on your back
- Nausea and vomiting
- Low grade fever
- Yellowing of the skin and eyes
- Rarely, shock—a medical emergency in which the organs and tissues don't receive adequate blood or fluids
Untreated acute pancreatitis can progress into chronic pancreatitis. This is a more serious condition that may lead to permanent damage of the pancreas. Chronic pancreatitis causes many symptoms, including:
- Abdominal pain
- Nausea and vomiting
- Weight loss
- Diarrhea
- Oily stools
- Mild diabetes
Diagnosis
You will be asked about your symptoms and medical history and a physical exam will be done. Your doctor may ask about your alcohol habits and what medications you take. Blood tests will help to make the diagnosis since certain enzymes are much higher in the blood with acute pancreatitis. The doctor also may need to take images of the pancreas to help show changes to the pancreas, gallstones, or any duct blockages. Images may be taken with:
- Abdominal ultrasound
- Abdominal CT scan
- Abdominal MRI scan
- Magnetic resonance cholangiopancreatography (MRCP)
The doctor will use information from all of the tests to make a diagnosis.
Treatment for Pancreatitis
Treatment depends on the severity of the pancreatitis and what is causing it. For example, if medication is the cause, your doctor may simply change the medication or the dose. The goal of treatment is to relieve pain, and manage nutritional and metabolic problems. Other treatment options include:
Prescription Medications
Your doctor may recommend medications like:
- Prescription pain relievers
- Pancreatic enzymes
- Vitamin supplements
- Medications to control diabetes if it develops
Lifestyle Changes
You may be advised to make lifestyle changes, such as:
- Eliminating alcohol, which may require counseling or a rehabilitation program. Stopping alcohol intake is the most important treatment intervention for chronic pancreatitis.
- Quitting smoking.
- Restricting the amount of fat in your diet. Pancreatic damage interferes with the body's ability to process fats. A registered dietitian can help create a healthy meal plan.
Hospitalization
The pancreas will begin to work anytime food and drink is taken. To allow the pancreas to fully rest, you will not be allowed to eat or drink. Fluids and other nutrition will be given until your condition is stabilized. Stabilization can be done with:
- Intravenous (IV) fluids
- Nasogastric tube—a long, thin tube that is threaded through the nose and into the stomach for feeding
Pancreatitis also can cause an imbalance in other enzymes and insulin. The medical team will give you medications to help manage these side effects until the pancreatitis has passed. In addition, if other treatment is needed to address the root cause of your pancreatitis, it will be done while you are in the hospital. Typically, the bout will pass in a few days with no lasting damage, though severe pancreatitis may take a few weeks to fully heal.
Surgery
Surgery may be needed for:
- Severe cases that do not respond well to rest
- Treating underlying conditions
Surgical options include:
- Percutaneous catheter drainage—thin tubes are inserted into the abdomen to drain fluid from the pancreas.
- Endoscopic retrograde cholangiopancreatography (ECRP)—used to remove gallstones or open any collapsed ducts.
- Cholecystectomy—used to remove the gallbladder and to reduce your chance of getting acute pancreatitis again.
- Necrosectomy—the removal of dying or dead pancreatic tissue.
Risk Factors
A risk factor is something that increases your chances of developing a certain condition. Risk factors for pancreatitis include:
- Gender—pancreatitis is more common in men
- Personal health history, such as:
- Excess alcohol intake
- Smoking
- Recurrent attacks of acute pancreatitis
- Family history of:
- Hyperparathyroidism associated with chronic pancreatitis
- Chronic pancreatitis
- Hypercalcemia
- Chronic kidney disease
- Congenital conditions (those present at birth)
- Ischemia—insufficient blood supply to the pancreas
- Hyperlipidemia—elevated blood fat levels
- Hypertriglyceridemia—elevated blood triglyceride levels
- Hypercalcemia—elevated blood calcium levels
- Cystic fibrosis
- Conditions that obstruct the passageway from the pancreas to the small intestine include:
- Trauma
- Tumors
- Pseudocysts—build up of fluids and debris
Chronic pancreatitis is a risk factor for developing pancreatic cancer.
Prevention
To help reduce your chance of getting acute pancreatitis, take these steps:
- Limit alcohol to a maximum of 2 drinks per day for men and 1 drink per day for women.
- If you have hyperlipidemia, restrict your intake of fat and follow your doctor’s treatment plan to lower your lipids.
- Increase your vegetable consumption.
- Increase your activity level to help lose excess weight. Aim for 30 minutes per day on most days of the week.
- Make sure your vaccinations are up to date, including mumps, rubella hepatitis B, and varicella.
- If you smoke, talk to your doctor about ways to quit. Smoking can irritate the pancreas.
- Avoid fatty meals. High amounts of fat intake put extra stress on the pancreas.
Additional resources can be found through the National Pancreas Foundation, www.pancreasfoundation.org.
If you are exhibiting symptoms of pancreatitis, please consult your physician. Dr. Shail Sheth, with Regional Health Gastroenterology can help with diagnosis and treatment. To schedule an appointment call the office at (812) 234-5400 or click below to book an appointment online.
Book An Appointment Online with